Several other disorders and conditions are associated with PWS. Some of the more common are obesity and secondary problems due to extreme obesity, diabetes (Type 2), sleep apnea, obsessive-compulsive disorder, infertility and autism-spectrum disorders.
As most of you know, Clementine was diagnosed with T1D (Type 1 Diabetes) when she was about 18 months old. This diagnosis is not linked to PWS and is simply an unrelated development. But boy, what a development! Prior to being diagnosed, we began to notice some signs typical of early stage diabetes. The signs were things like excessive thirst (it’s VERY unusual for someone with PWS to consume a lot of liquids unless the liquid is sweet) , lethargy and weight loss. Because I had recently had a family member develop T2D, which has the same warning signs, I knew what I was seeing. Even so, it did take a while to really put things together. What finally did the trick was when my husband was giving Clem a bath and he called me in to look at her. She was experiencing “diabetic wasting” and had lost a good bit of weight. Her ribs were prominent and she looked very frail. As I was looking at her poor little body, it hit me like a lightening bolt… she has diabetes.
Stephan and I talked about it and decided that this must be what was going on. I called our pediatrician and we went into his office the following day. I explained the symptoms and my concerns to him. He was doubtful that diabetes was what we were seeing but he had her blood sugar tested. Bingo! Her blood sugar levels were about 400. Just as a gauge, normal pediatric blood sugar levels range from 80 to 150. The next thing I knew, we were in an ambulance, heading to Children’s Healthcare of Atlanta.
Once at the hospital, testing was done to officially diagnose T1D. Sure enough, the antibodies test came back positive. Antibodies are produced in someone with diabetes because the immune system is attacking the pancreatic beta cells and this results in antibody production. The hospital staff, when learning of our self diagnosis and insistence upon testing by our pediatrician, were amazed. Several of them told me that we were very lucky to have caught this so early on. Most kids don’t come in for testing until they reach a much higher level of DKA (diabetic ketoacidosis) and are quite ill. The normal blood sugar level for kids being admitted under these circumstances is above 800. So even though Clem was admitted at 400, we were well ahead of the curve. I guess that was something to be thankful for!
As the news that Clem had T1D sank in, I kept thinking to myself, well if she has to have something else, it could be much worse. This turn of events didn’t really shake me as much as it could have. I guess after the shock of being diagnosed with PWS, everything else that happens is less monumental. I called Dr. Miller, Clem’s PWS specialist, and she was very surprised to hear the news. She told me that T1D is rare in PWS patients and that she had only a handful out of her 500 plus patients that had both conditions.
T2D is much more common in PWS persons, primarily because of obesity. I’m always taken aback when people think that T1D and T2D are the same. They are not. T1D is an autoimmune disease that destroys the body’s ability to make insulin and control blood sugar levels. All T1 diabetics will become insulin dependent within a short time of diagnosis. The true origin of T1D isn’t fully understood and there is no cure. Management is complex and time consuming and requires diet control and proper physical activity. There are significant long term health risks associated with poorly managed diabetes. Risks like heart disease, stroke, kidney failure, retinopathy and poor circulation. In fact, diabetic complications are the number 1 reason for limb amputation in the US!
T2D is a condition that causes the body to fail to recognize and to efficiently use its own insulin. It is typically brought on by obesity, sedentary habits and poor diet. Usually T2D can be managed by proper diet, exercise and weight loss. Many people with T2D can refrain from becoming insulin dependent if they utilize the appropriate lifestyle tools. The biggest difference between the 2 conditions is that T1 diabetics don’t produce their own insulin and T2 diabetics still produce their own insulin.
Anyway, when it became known that Clem was a T1D, I quickly realized that this would bring her health challenges to a whole new level of complexity. Strangely enough, I felt as if these 2 conditions fit together nicely. We were already on the path to strict dietary restrictions because of PWS so adding T1D just made it all the more important. And because Clem was so young, she would never remember a time when she didn’t have dietary restrictions. It would all seem natural to her.
Post diagnosis, we struggled to find a good local pediatric endocrinologist for Clem. There were plenty of them but none had experience with both conditions in 1 patient. After having a few poor experiences, I called Dr. Miller in frustration. While we were talking, I had an idea. What if I could see someone in her department that specialized in T1D? I asked her who she would see if it was her daughter. Her immediate response was Dr. Des Schatz. Dr. Miller contacted him on our behalf and even though he wasn’t accepting new patients, he agreed to see us.
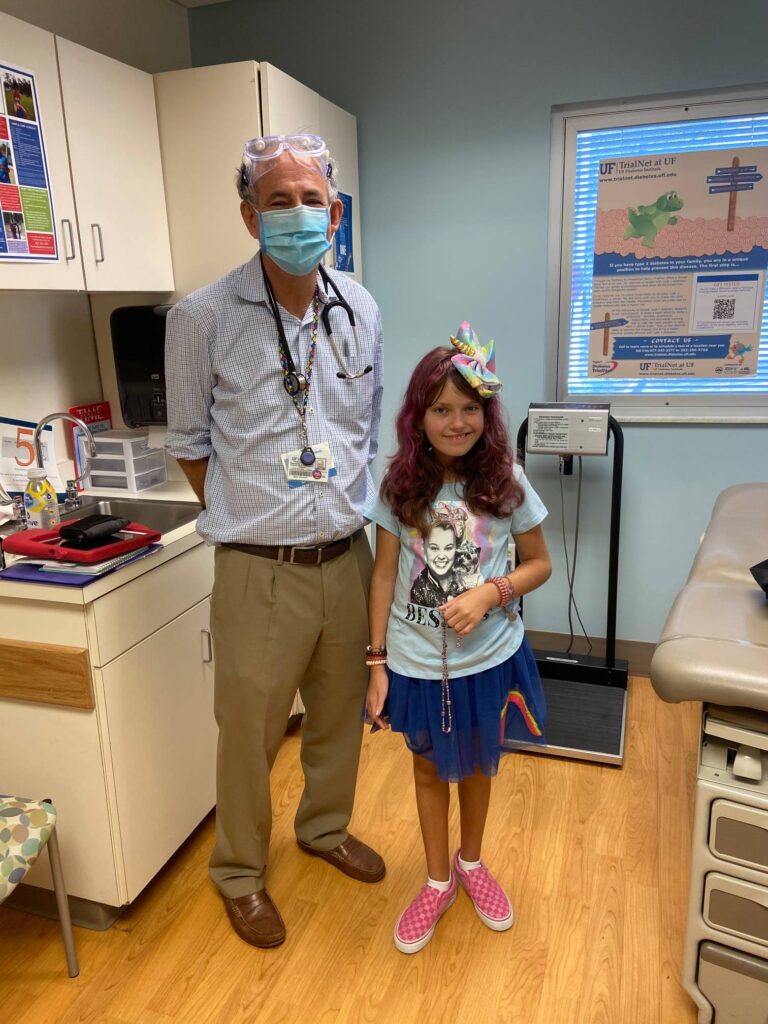
Off we went to Gainesville. At our first meeting, Dr. Schatz quizzed me on my T1D knowledge. He listened to Dr. Miller talk about the potential problems she thought we might experience because of our dual diagnosis. I must have passed his test because he agreed to take on Clem’s diabetic care. Dr. Des assured me that together we could manage Clem’s situation and he gave me hope that it would all be ok. Now I had the dream team and Clem’s care was brought to the highest level possible.
Through the following years, we have experienced many ups and downs related to T1D. Diabetes is very difficult to manage in kids because blood glucose levels are influenced by many factors, most of which can’t be controlled. Diet, exercise and weight control are the only things one can really manage externally. The other factors, things like illness, physical growth and natural physiological functions are out of reach of my influence. Stress is another factor and one that is tied to PWS. Clem has high levels of anxiety caused by PWS and this does make her diabetes more volatile. Medications also have an effect of blood glucose levels, particularly growth hormone. Clem receives a high dose of GH every night and it causes her BGs to rise. This isn’t a solvable situation. We manage it the best we can with precise insulin dosing and constant monitoring.
When Clem became a patient of Dr. Des, he asked me why she wasn’t using an insulin pump. I had tried to convert to a pump with our previous endos but was turned down because of Clem’s age and because of her PWS diagnosis. Dr. Des thought that was ridiculous so we started using a pump right away. She was 3. The closed loop system was developed and put on the market when Clem was around 7. This system incorporates both a continuous glucose monitor and an insulin pump to manage blood glucose. When they first arrived on the market, they were not recommended for kids under the age of 12. But Dr. Des, who was confident that we could manage the system, allowed us to begin using it and it has really made a big difference. Just 2 months ago, we upgraded to an improved “artificial pancreas system” and although it has some blue tooth issues, it’s working great! Diabetes technology has come a long way. There are many more advances on the horizon.
After more than 10 years as a diabetic, Clem handles all of the issues and restrictions that come with T1D very well. She tolerates her pump and CGM and never complains about having to wear them. She has finally come to recognize the signs of both high and low blood sugars (when she was younger she suffered from hypoglycemic unawareness, which is when the body doesn’t produce the right warning signs or the signs are not perceived) and she clearly communicates these sign to us. Clem understands the seriousness of having diabetes and she is able to teach others about the condition.
I would be lying if I said diabetes is easy. It most certainly isn’t. In fact, it can be more difficult to manage on a day to day basis than PWS. The complications from diabetes symptoms can be deadly and can be immediate. Extreme hypoglycemia can cause death within a short period of time. The effects of PWS on physical health are mostly cumulative.
As with all other things, we simply deal with what is and move forward. At present, neither T1D nor PWS is curable. Both are manageable to degrees but both require much more research to fully understand and to conquer. I will be raising money for T1D later this year. But for now, we are focusing on PWS fundraising.